Sleep Smarter, Spot Trouble Early: My Real Routine That Changed Everything
You know that groggy, drained feeling even after eight hours of sleep? I lived with it for years—until I realized my restless nights weren’t just about fatigue. Poor sleep was masking early signs of health issues I couldn’t ignore. Turns out, how we sleep doesn’t just affect energy—it can signal deeper problems. This is how tuning into my sleep patterns helped me catch red flags early, feel truly refreshed, and take real control of my well-being—naturally and sustainably. What began as a simple desire to wake up feeling better evolved into a journey of self-awareness, prevention, and lasting health transformation.
The Hidden Language of Sleep: When Tiredness Is More Than Tiredness
For many women in their 30s, 40s, and beyond, fatigue is often brushed off as a normal part of life. Between managing households, careers, and family needs, exhaustion can seem inevitable. Yet chronic tiredness, even after what appears to be a full night’s rest, is not a badge of honor—it may be a whisper from the body trying to communicate something deeper. Sleep disturbances such as waking up multiple times, difficulty falling asleep, or feeling unrested despite adequate time in bed are not just inconveniences. They can be early indicators of underlying physiological imbalances.
Research has shown that disrupted sleep patterns may precede more serious health concerns by months or even years. For instance, frequent nighttime awakenings have been associated with early signs of hormonal shifts, particularly during perimenopause, when fluctuations in estrogen and progesterone can directly impact sleep architecture. Similarly, unrefreshing sleep has been linked to metabolic issues such as insulin resistance, a precursor to type 2 diabetes. These connections are not speculative; they are grounded in clinical observations and longitudinal studies tracking sleep and health outcomes.
Another often-overlooked signal is the combination of fatigue and brain fog. Many women report struggling with focus, memory lapses, or low motivation, assuming these are simply stress-related. However, when paired with poor sleep, these symptoms may point to thyroid dysfunction or chronic inflammation. Sleep is a restorative process, and when it is repeatedly interrupted, the body lacks the time it needs to repair tissues, regulate hormones, and clear metabolic waste from the brain.
The key is not to jump to conclusions or self-diagnose, but to become an observer of one’s own patterns. Just as a car’s dashboard light doesn’t mean the engine is ruined, but signals the need for inspection, sleep disruptions serve as an early warning system. Recognizing them as such shifts the mindset from resignation to responsiveness. Instead of accepting fatigue as inevitable, women can begin to ask: What is my body trying to tell me? This shift in perspective is the first step toward proactive health management.
Why Sleep Quality Matters More Than Sleep Quantity
Spending eight hours in bed does not automatically equate to eight hours of restorative sleep. What truly matters is the quality of those hours—the depth, continuity, and balance of sleep stages. A night filled with light, fragmented sleep may leave someone physically in bed but mentally and physiologically unrefreshed. This is because the body cycles through distinct phases: light sleep, deep sleep, and REM (rapid eye movement) sleep, each playing a unique role in health.
Deep sleep, often called slow-wave sleep, is when the body repairs muscles, strengthens the immune system, and restores energy. Growth hormone is primarily released during this stage, supporting tissue regeneration and metabolic balance. Disruptions in deep sleep—caused by stress, noise, or medical conditions like sleep apnea—can impair these essential functions. Over time, this sets the stage for chronic inflammation, a known contributor to heart disease, arthritis, and other long-term conditions.
REM sleep, on the other hand, is critical for cognitive health. It supports memory consolidation, emotional regulation, and mental clarity. When REM cycles are shortened or delayed due to alcohol consumption, medication, or anxiety, individuals may wake up feeling emotionally raw or mentally sluggish. Studies have shown that REM deprivation can mimic symptoms of mood disorders, even in otherwise healthy individuals.
One way to assess sleep quality is through morning markers. Do you wake up naturally, or do you rely heavily on an alarm? Do you feel alert within 30 minutes of rising, or do you need multiple cups of coffee to function? Is your mood stable throughout the day, or do you experience unexplained irritability or fatigue? These are practical, everyday indicators that offer more insight than any single night’s duration. Tracking these patterns over time can reveal trends that hint at deeper issues—long before clinical symptoms appear.
Additionally, poor sleep quality has been linked to elevated cortisol levels, the body’s primary stress hormone. When cortisol remains high at night, it interferes with melatonin production, making it harder to fall and stay asleep. This creates a vicious cycle: poor sleep increases stress, and stress further degrades sleep. Breaking this cycle requires more than just trying to sleep longer—it demands a focus on creating the right internal and external conditions for high-quality rest.
My Sleep Upgrade: Simple Tweaks That Actually Worked
My turning point came when I stopped chasing sleep and started supporting it. I had tried everything—sleeping pills, herbal teas, blackout curtains—but nothing delivered lasting results. What finally made a difference wasn’t a miracle cure, but a series of small, consistent changes grounded in science and personal experimentation. The first was setting a fixed bedtime and wake-up time, even on weekends. This may sound basic, but it was revolutionary for my body’s internal clock. Within two weeks, I noticed I was naturally feeling sleepy around 10 p.m. and waking closer to 6 a.m. without an alarm.
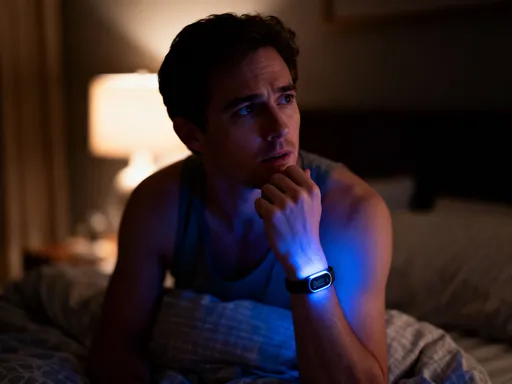
The second change was reducing blue light exposure after sunset. I began turning off overhead lights and switching to warm-toned lamps in the evening. More importantly, I committed to no screens—no phones, tablets, or television—after 8:30 p.m. Blue light suppresses melatonin, the hormone that signals it’s time to sleep. By eliminating this interference, my body began producing melatonin earlier, making it easier to fall asleep without lying awake for hours.
I also created a wind-down ritual that didn’t involve screens. Instead of scrolling through social media, I spent 30 minutes reading a physical book, journaling, or doing gentle stretching. This transition period helped my nervous system shift from “on” to “off,” reducing mental chatter and preparing my body for rest. I discovered that consistency mattered more than perfection. Even on busy nights, doing just 10 minutes of quiet activity made a difference.
Dietary adjustments played a role too. I stopped drinking coffee after 2 p.m., realizing that even if I felt fine in the evening, caffeine’s half-life meant it was still active in my system at bedtime. I also reduced heavy meals and alcohol in the evening, both of which can fragment sleep. Instead, I opted for light, balanced dinners with protein and complex carbohydrates, which supported stable blood sugar overnight.
Within a month, the changes were undeniable. I woke up feeling more alert, my mood was more stable, and I had sustained energy throughout the day. I wasn’t just sleeping more—I was sleeping better. The most surprising benefit was mental clarity. Tasks that used to feel overwhelming became manageable. This wasn’t due to any drastic overhaul, but to the cumulative effect of small, sustainable habits that honored my body’s natural rhythms.
Listening to Your Body: Recognizing Early Warning Signs
One of the most empowering aspects of improving sleep has been learning to listen to my body. Subtle changes—like waking up at the same time every night, experiencing night sweats, or noticing new snoring—can be early clues to physiological shifts. For example, waking between 2 and 3 a.m. repeatedly may be linked to blood sugar fluctuations or liver function, especially if accompanied by hunger or anxiety. Night sweats, often dismissed as hormonal, can also signal thyroid imbalances or chronic stress.
Snoring, particularly if it’s a new development, should not be ignored. While occasional snoring can be harmless, persistent or loud snoring may indicate obstructive sleep apnea, a condition where breathing pauses during sleep. This not only disrupts rest but also increases strain on the cardiovascular system. Many women don’t recognize the signs because apnea presents differently in women than in men—more often as fatigue, insomnia, or mood changes rather than loud snoring.
To track these patterns, I started a simple sleep journal. Every morning, I noted how I felt upon waking, any disturbances during the night, and lifestyle factors like caffeine, alcohol, or stress levels. Over time, patterns emerged. I noticed that higher stress days led to more fragmented sleep, and late meals correlated with restlessness. This wasn’t about perfection—it was about awareness. The journal became a tool for early detection, helping me identify trends before they became problems.
It’s important to distinguish between temporary disruptions and persistent patterns. Life events—travel, illness, family stress—can temporarily affect sleep, and that’s normal. But when poor sleep lasts more than a few weeks, or when new symptoms arise, it’s time to consult a healthcare provider. Early medical evaluation can rule out or address underlying conditions such as anemia, thyroid disorders, or sleep apnea. The goal isn’t to pathologize every bad night, but to recognize when patterns suggest the need for professional insight.
Listening to your body also means honoring its signals without judgment. Instead of criticizing myself for waking up, I began asking: What does this mean? Is it stress? Hormonal change? A dietary trigger? This mindset shift—from frustration to curiosity—transformed my relationship with sleep. It became less of a battle and more of a dialogue with my body.
The Power of Routine: Building a Sleep-First Lifestyle
Sleep doesn’t exist in isolation—it’s deeply connected to daily rhythms. A sleep-first lifestyle means aligning daily habits with the body’s natural circadian clock. One of the most effective strategies I adopted was morning sunlight exposure. Within 30 minutes of waking, I made it a habit to step outside, even for just 10 minutes. Natural light helps regulate melatonin and cortisol, reinforcing the body’s internal clock and improving sleep onset at night.
Physical activity also plays a crucial role. Regular movement, especially in the morning or afternoon, supports deeper sleep by reducing stress and promoting physical tiredness. However, intense exercise too close to bedtime can be stimulating for some, so I shifted my workouts earlier in the day. Even a 20-minute walk after dinner helped digestion and eased the transition into evening calm.
Meal timing became another key factor. Eating dinner at least three hours before bed allowed my body to digest fully, reducing the risk of acid reflux or discomfort at night. I also avoided late-night snacks, which can spike insulin and disrupt sleep cycles. Instead, if I felt hungry, I opted for a small portion of protein or healthy fat, like a handful of almonds or a slice of turkey, which stabilized blood sugar without overloading the digestive system.
Equally important was managing mental load. I stopped making big decisions or engaging in emotionally charged conversations after 8 p.m. The brain needs time to wind down, and late-night stress keeps cortisol elevated. I created a buffer zone between daily responsibilities and bedtime, using the hour before sleep for calming activities. This wasn’t about adding more tasks, but about protecting the transition into rest.
Consistency, not perfection, was the foundation. I allowed flexibility for weekends or special events, but maintained a core routine that gave my body predictability. Over time, this rhythm became second nature. My body began to anticipate bedtime, making it easier to fall asleep and stay asleep. A sleep-first lifestyle isn’t about rigid rules—it’s about creating a supportive environment where rest can thrive.
Tools Without Hype: What Actually Helps (And What Doesn’t)
The market is full of sleep gadgets promising better rest, but not all deliver meaningful results. After trying several, I learned to separate evidence-based tools from marketing hype. One device that provided real value was a simple sleep tracker worn on the wrist. It didn’t give perfect data, but it revealed trends—like how often I woke up, how much deep sleep I got, and how lifestyle choices affected my rest. Seeing that late caffeine reduced my deep sleep by 20% was a powerful motivator to change habits.
White noise machines were another helpful addition. For those sensitive to environmental noise—traffic, household sounds, or a partner’s movements—consistent background sound can reduce nighttime awakenings. I found that nature sounds or pink noise worked better than music, which can be stimulating. The key was using it consistently, not as a fix but as a supportive element.
On the other hand, I found little benefit in expensive mattresses or specialized pillows, despite their claims. While comfort matters, there’s limited evidence that high-end bedding significantly improves sleep quality for most people. Similarly, supplements like melatonin should be used cautiously. Short-term use may help reset a disrupted clock, but long-term reliance can reduce the body’s natural production. I now reserve melatonin for travel or occasional disruptions, not as a nightly crutch.
Apps that promise sleep coaching or meditation can be useful, but only if they’re part of a broader routine. Relying solely on a 10-minute meditation to fix chronic sleep issues is unrealistic. The most effective tools are those that provide insight and encourage behavior change, not those that offer quick fixes. The goal is not dependency on gadgets, but empowerment through awareness.
From Awareness to Action: Making Sleep a Health Priority
Improving sleep transformed more than just my energy levels—it changed how I view health. Sleep is no longer something I sacrifice for productivity; it’s a non-negotiable pillar of well-being. Research increasingly shows that sleep is a vital sign, just like blood pressure or heart rate. It reflects the state of the body’s systems and can signal imbalances long before traditional symptoms appear.
By treating sleep as a diagnostic window, I’ve been able to catch potential issues early and take preventive action. This proactive approach has given me a sense of control and confidence in my health journey. It’s not about fear or obsession, but about respect for the body’s intelligence. When we listen, it tells us what it needs.
Sustainable change comes from small, consistent choices—not overnight transformations. The habits I’ve adopted are simple, science-backed, and adaptable to real life. They don’t require expensive products or drastic lifestyle overhauls. What they do require is attention, intention, and a willingness to prioritize rest as an act of self-care.
For women juggling multiple roles, sleep can feel like the first thing to give up. But the truth is, everything else suffers when sleep does. Energy, mood, focus, immunity—all depend on quality rest. By making sleep a priority, we invest in our long-term health, resilience, and quality of life. The journey begins not with perfection, but with awareness. And from there, real change becomes possible.